The addicted brain
(This article was first printed in the July 2004 issue of the Harvard Mental Health Letter. For more information or to order, please go to www.health.harvard.edu/mental.)
Drug addiction has been a stubborn problem for thousands of years, but only in the last generation have scientists come to understand clearly one of the reasons: It causes lasting changes in brain function that are difficult to reverse. That means many altered brains �?nearly 2 million heroin and cocaine addicts, perhaps 15 million alcoholics, and tens of millions of cigarette smokers in the United States alone. No simple solution is in sight, but we know much more than we did 20 or even 5 years ago about how the brain responds to addictive drugs, and that knowledge is beginning to affect treatment and prevention.
Why does the brain prefer opium to broccoli?
The question of addiction has been put that way by Steven Hyman, a former director of the National Institute of Mental Health. The answer involves the nucleus accumbens, a cluster of nerve cells that lies beneath the cerebral hemispheres. When a human being or other animal performs an action that satisfies a need or fulfills a desire, the neurotransmitter dopamine is released into the nucleus accumbens and produces pleasure. It serves as a signal that the action promotes survival or reproduction, directly or indirectly. The system is called the reward pathway. When we do something that provides this reward, the brain records the experience and we are likely to do it again. Damage to the nucleus accumbens and drugs that block dopamine release in the region make everything less rewarding.
In nature, rewards usually come only with effort and after a delay. Addictive drugs provide a shortcut. Each in its own way sets in motion a biological process that results in flooding the nucleus accumbens with dopamine. The pleasure is not serving survival or reproduction, and evolution has not provided our brains with an easy way to withstand the onslaught. In a person who becomes addicted through repeated use of a drug, overwhelmed receptor cells call for a shutdown. The natural capacity to produce dopamine in the reward system is reduced, while the need persists and the drug seems to be the only way to fulfill it. The brain is losing its access to other, less immediate and powerful sources of reward. Addicts may require constantly higher doses and a quicker passage into the brain. It’s as though the normal machinery of motivation is no longer functioning; they want the drug even when it no longer gives pleasure.
The brain’s reward system 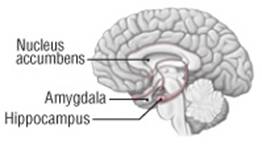
Addictive drugs provide a shortcut to the brain’s reward system by flooding the nucleus accumbens with dopamine. The hippocampus lays down memories of this rapid sense of satisfaction, and the amygdala creates a conditioned response to certain stimuli. Stressors or something associated with substance use can trip the mental machinery of relapse. |
Compelling memories
Changes in the reward system alone cannot explain why addiction persists. As Mark Twain said of his tobacco habit, quitting is easy; he had done it often. Many addicts go through long periods without taking the drug, but they risk relapse even after years of abstinence, when the dopamine reward circuit has had plenty of time to recuperate. They are victims of conditioned learning, which creates habitual responses.
Drug-induced changes in the links between brain cells establish associations between the drug experience and the circumstances in which it occurred. These implicit memories can be retrieved when addicts are exposed to any reminder of those circumstances �?moods, situations, people, places, or the substance itself. A heroin addict may be in danger of relapse when she sees a hypodermic needle, an alcoholic when he passes a bar where he used to drink or when he meets a former drinking companion. Any addict may resume the habit on falling into a mood in which he used to turn to the drug. A single small dose of the drug itself is one of the most powerful reminders �?“It’s the first drink that gets you drunk,�?as they say in Alcoholics Anonymous.
Internal or external stress is another cause of relapse. The nucleus accumbens sends signals to the amygdala and hippocampus, which register and consolidate memories that evoke strong feelings. When asked why they relapse, addicts may say, “My job was not going well,�?or even, “The traffic was so heavy that day.�?These answers suggest that they are hypersensitive to stress, either congenitally or as a result of past addiction. Levels of corticotropin releasing hormone (CRH), the brain chemical that regulates the stress hormone system, often rise in addicts just before a relapse, while the amygdala becomes more active. Mice bred without receptors for CRH are less susceptible to drug addiction.
In the last few years, research has suggested that addiction involves many of the same brain pathways that govern learning and memory. Addiction alters the strength of connections at the synapses (junctions) of nerve cells, especially those that use the excitatory neurotransmitter glutamate. Underlying these changes are drug-induced activation and suppression of genes within nerve cells, another process scientists are beginning to explore.
Why we are not all addicted
The reward system may be more vulnerable, responses to stress more intense, or the formation of addictive habits quicker in some people, especially those suffering from depression, anxiety, or schizophrenia, and those with disorders like antisocial and borderline personality.
Twin and adoption studies show that about 50% of individual variation in susceptibility to addiction is hereditary. Mice with an extra gene for the production of a certain nerve cell protein are more vulnerable to cocaine addiction. According to a recent report, one gene variant reduces the amount of dopamine release caused by cocaine in human beings �?a genetic defense against at least one type of addiction.
Individuals also differ in their capacity to exercise judgment and inhibit impulses. The brain’s prefrontal cortex helps to determine the adaptive value of pleasure recorded by the nucleus accumbens and checks the urge to take the drug when it would be unwise. If the prefrontal cortex is not functioning properly, an addictive drug has more power to monopolize the reward circuit. Recent research shows that the prefrontal cortex is not fully developed in adolescence, which could explain why we so often develop addictions at that time of life. (A person who does not become a smoker before age 21 will probably never be addicted to nicotine.) Antisocial personalities also have deficiencies in prefrontal functioning.
Implications for prevention and treatment
Although findings on the addicted brain are suggesting new approaches to treatment, progress has been limited so far. Researchers have tested dopamine receptor antagonists, drugs that bind to receptors for dopamine and prevent addictive drugs from acting. But these substances usually have too many side effects because they also interfere with the motivation for natural and adaptive rewards. One way to avoid side effects is to disrupt the mechanisms by which individual drugs start the process that culminates in dopamine release; for example, the opiate antagonist naltrexone is now used to treat both heroin addicts and alcoholics.
The biggest problem is preventing relapse. Neutralizing the pleasurable effect of the drug is not enough because reminders of the drug experience perpetuate the longing and cause addicts to stop taking the counteracting medication. Glutamate has been the main target of research on relapse prevention. In one experiment, formerly addicted rats returned to using cocaine when their hippocampi �?the brain region where memories of the drug experience are likely stored �?were electrically stimulated. A drug that blocked glutamate activity prevented this re-addiction.
An all-out assault on glutamate is impossible. Half the neurons in the cerebral cortex use this transmitter, and a major reduction in its activity would be toxic. Instead, researchers are trying to target specific types of glutamate nerve receptors in specific parts of the brain. Acamprosate, used in the treatment of alcoholism, acts at the NMDA receptor, a type of glutamate receptor. The anticonvulsant topiramate (Topamax), another proposed medication for alcoholics, may also act at that receptor. Memantine, a relatively new drug that blocks NMDA receptors, has proved promising in one small study of heroin addicts.
Researchers are working on other approaches to medication for addictive disorders. Some are looking into the possibility of preventing stress-induced relapse by blocking the activity of CRH. Others are experimenting with immunization for cocaine and nicotine �?training the immune system to recognize the drug by injecting a molecule that simulates its effect, creating antibodies with the capacity to break the drug down before it reaches the brain.
What is substance dependence? A diagnosis of substance (drug) dependence requires at least three of the following: - Tolerance: getting less effect with continued use of the same amount of the drug, or needing higher doses to get the same effect, or both.
- Suffering withdrawal symptoms, and using the drug to relieve them.
- Taking more of the drug than intended or for a longer time than intended.
- Persistently wanting to �?or unsuccessfully trying to �?cut down or control drug use.
- Spending a great deal of time obtaining the drug, using it, or recovering from its effects.
- Giving up other important activities as a result of or for the sake of drug use.
- Continuing to use the drug even though it causes serious physical or psychological harm.
Adapted from the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision, 2000. |
The old and the new
The more scientists learn about addiction, the clearer it becomes that chemical solutions will not be available soon. For the foreseeable future, medications will be only an aid to psychosocial treatment. We will still need 12-step self-help groups, behavioral therapies, and exploration of traumatic and everyday experiences that may have disturbed the balance of the reward and inhibition system or the process of learning by association.
Behavior therapy provides sources of reward and punishment that compete with the drug, such as payment for clean urine in the form of vouchers, or contingency contracts (in which addicts agree to give up something important to them if they go back to using the drug). Behavior therapists also work to change the learned associations that create the risk of relapse.
Motivation or will can be regarded as a brain function that is damaged by addiction, just as language or movement can be damaged by a stroke. In successful treatment of a stroke, other parts of the brain assume the functions of the injured region. In the same way, treatment for addiction may be able to make use of the remaining healthy parts of the motivation system to repair the damage. Twelve-step groups and motivational enhancement therapy could be seen as ways of accomplishing that.
Treatment will always depend on the type of addiction and the type of addict. Novelty seekers and risk takers with insufficient inhibition and judgment will not necessarily respond to the same methods that work for people afflicted by traumatic stress or hypersensitivity to everyday stress. And the most important lesson of all in recent discoveries may be that addictions are chronic conditions for which there are treatments but rarely simple cures.
By identifying the nerve receptors that addictive drugs target, science has taught us much about both their individual and their common effects. But there is still much to learn about how changes in reward circuits lead to addiction, how the brain creates the unconscious memories that make addicts susceptible to relapse, why some people are especially vulnerable to addiction, and how to translate the knowledge we have into more effective treatments.
The new brain research suggests that addiction is not just a property of certain drugs but an aspect of certain human activities and relationships. Researchers have already found resemblances between the brain scan images of compulsive gamblers and drug addicts. The idea of addiction to television, video games, overeating, or sexual behavior may be more than a metaphor. Exploring the biology of addiction could lead to a deeper understanding of the sources of all human motivation and habit formation.
Source:
http://www.health.harvard.edu/newsweek/The_addicted_brain.htm
 Free Forum Hosting
Free Forum Hosting